
Our objectives were to identify among patients who underwent ablation treatment for AF at Mayo Clinic the occurrence of structural or functional complications in upper gastrointestinal (UGI) tract, to appraise clinical outcomes, review the association with vagal dysfunction, the probable mechanism of the functional UGI complication. Some of these limitations are overcome in a single center study especially if the sample size is large and the methods of treatment and diagnosis are standardized. 13 However, there are limitations of such survey-based data with limited follow-up, and the methods of diagnosis for functional gastrointestinal (GI) complications such as gastroparesis are not standardized in such multi-center studies. 10- 12 A recent multinational survey documented the incidence, clinical course over a short follow up period, and outcomes.
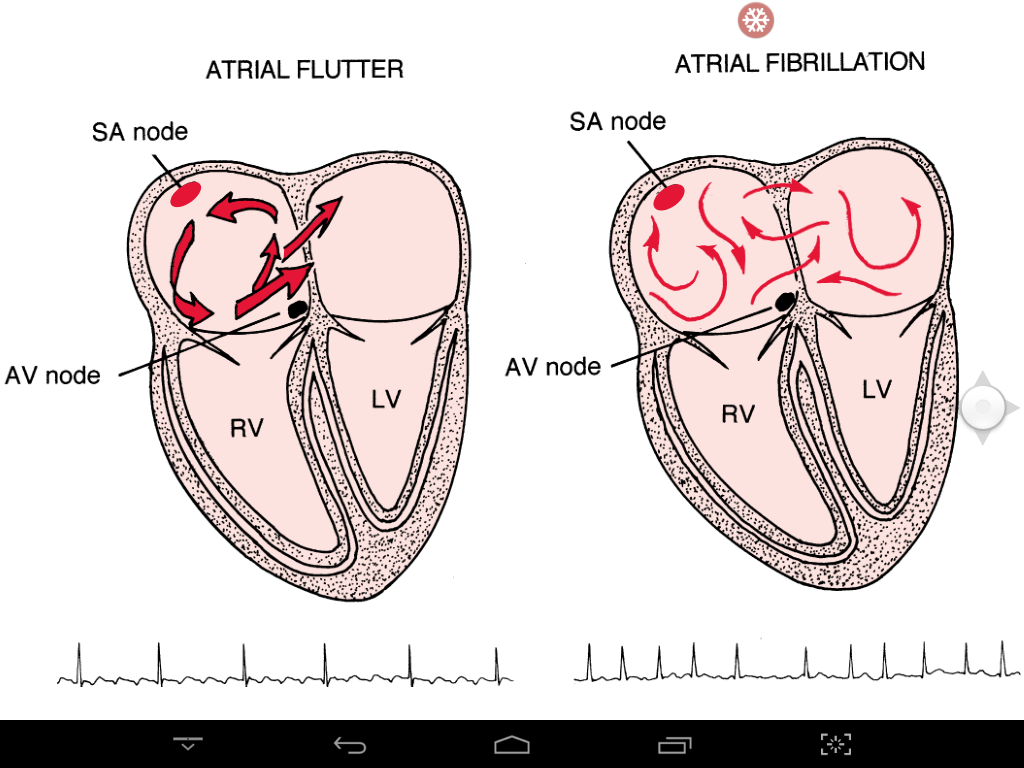
8, 9 Therefore, vagus nerve injury resulting from ablation therapy for AF may rarely lead to motor disorders such as gastroesophageal reflux and gastric hypomotility as a result of the dysfunction or injury of the vagus nerve. The periesophageal vagus nerve plexus supplies parasympathetic control to the motor functions of the stomach, digestive tract, and gallbladder. Thus, the vagus nerve and its branches are anatomically close to the posterior wall of the left atrium and the pulmonary vein, and may be injured during ablation treatment required to normalize cardiac arrhythmias such as atrial fibrillation. 5 There are many vagal nerve fibers (shown in yellow) that cross the esophagus close to the regions relevant to ablation of bundles of conducting fibers in the left atrium. The positions of the left atrium, trachea and main stem bronchi, esophagus, and vagus nerve are shown.


 0 kommentar(er)
0 kommentar(er)
